Dentistry Designed for Your Whole Body
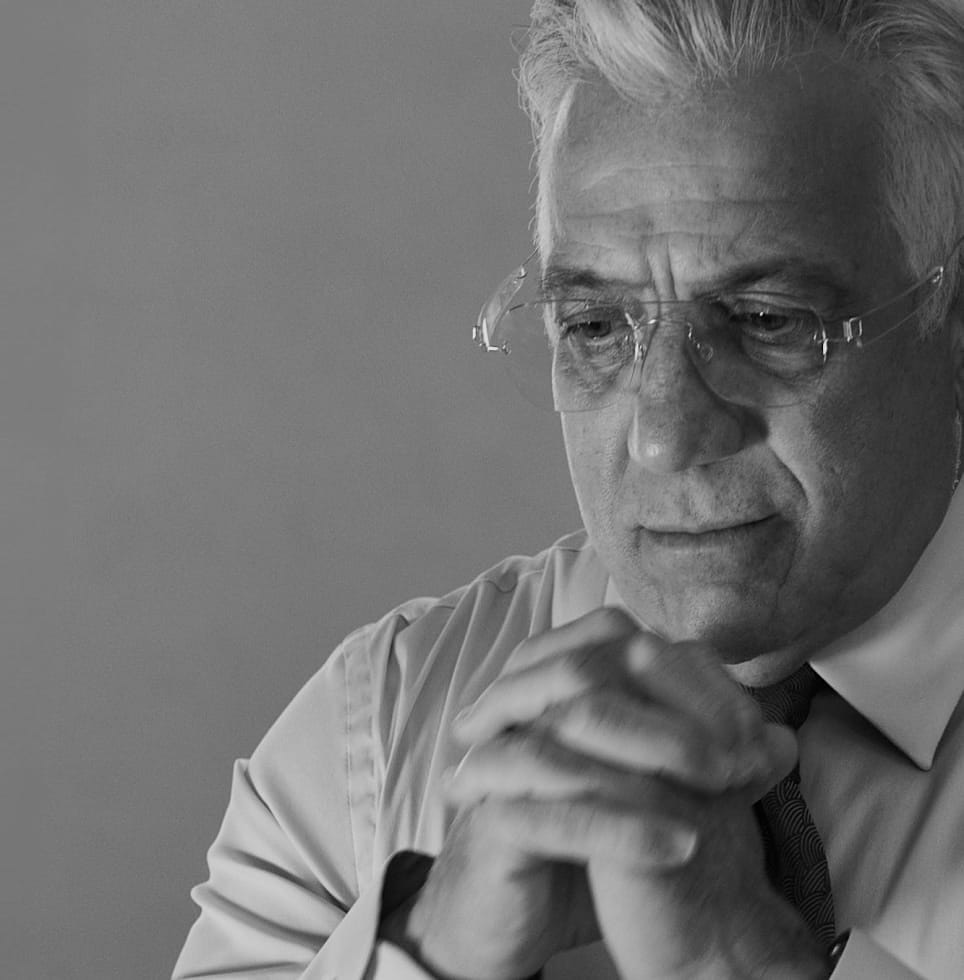
Dr. Gerry Curatola Fifth Avenue, New York & East Hampton Restorative Biological and Cosmetic Dentistry


Today, We Celebrate 40+ Years of Innovation
The Father of Modern Biologic Dentistry Redefining Oral Health and Wellness Through Holistic Innovation


Rejuvenation Dentistry News & Media
As Seen On Trusted by Professionals Worldwide
From pioneering biologic dentistry to promoting the critical connection between oral and systemic health, Dr. Curatola’s expertise has been spotlighted by top media outlets for his revolutionary approach to oral health, earning trust and recognition worldwide.

Dr. Curatola’s Handpicked Experts








Lasting Beauty is Built on Lasting Health
At Rejuvenation Dentistry, everything we do is with a biologic lens. A focus on overall oral health and the body’s natural biological processes always comes first, and our goal is to enhance the appearance of a patient’s smile while also taking into account the long-term health and well-being of the teeth and surrounding oral structures. The Rejuvenation approach recognizes the interplay between aesthetics and biology in dentistry.
Biologic Procedures
Experience dentistry that prioritizes your health. Our biologic procedures leverage non-toxic materials and holistic techniques to protect your oral microbiome, address root causes, and support overall wellness.

Cosmetic Procedures
Transform your smile with cosmetic treatments designed to enhance both beauty and function. From veneers to teeth whitening, our advanced techniques deliver natural, stunning results.

Restorative Procedures
Restore your smile and confidence with cutting-edge restorative dentistry. Our biologic dental implants, crowns, and bridges offer durable, aesthetically pleasing solutions that support long-term oral health.

Oral Surgery
Our oral surgery solutions, including cavitation treatment and bone grafting, provide advanced care tailored to your specific needs, ensuring a seamless journey to recovery and optimal health.